Untangling the cytokine storm - a supercomputer look at COVID-19
Earlier this summer, the SUMMIT supercomputer at Oak Ridge National Lab in Tennessee started crunching data on more than 40,000 genes from 17,000 genetic samples in an effort to better understand Covid-19. Despite being the world's second-fastest supercomputer, it took SUMMIT more than a week to analyze the approximately 2.5 billion genetic combinations — but it was worth the wait.
Once the analysis by SUMMIT was done, researchers from the team of Dr. Daniel Jacobson, lead researcher and chief scientist for computational systems biology at Oak Ridge, looked at the results.The results were striking and pointed towards a new "victim" of SARS-CoV-2 action - the bradykinin pathway. The bradykinin hypothesis provides a new model that explains many aspects of Covid-19, including some of its most bizarre symptoms. It also suggests several potential treatments, many of which are already FDA approved. Jacobson’s group published their results in a paper in the journal eLife in early July.
From ACE2 to the bradykinin pathway
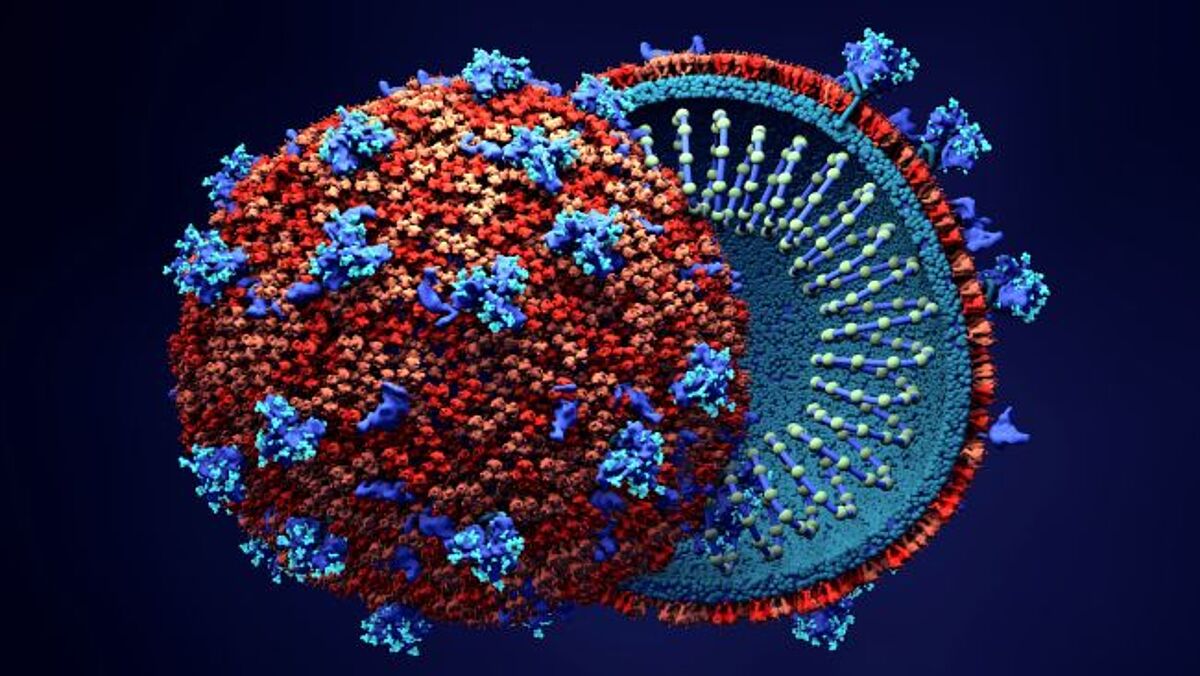
COVID-19 infection generally begins when the virus enters the body through ACE2 receptors, which are particularly abundant in the nose. The virus then moves through the body, entering other ACE2-expressing cells: the intestines, kidneys, and heart, for example. Infection of these tissues and the ensuing cellular damage likely account for at least some of the disease’s cardiac and GI symptoms.
According to Jacobson’s group, SARS-CoV-2 then starts hijacking other pathways, such as the renin–angiotensin system (RAS), which controls many aspects of the circulatory system, including the body’s levels of bradykinin. This hormone normally helps to regulate blood pressure and when the virus starts interfering with RAS, it has a tremendous effect on bradykinin levels. Consequently, bradykinin receptors are re-sensitized, and the body stops breaking down bradykinin. The result of these action is effectively a bradykinin storm and it may be this storm which is ultimately responsible for many of the clinical complications seen in SARS-CoV-2 infection.
For example, recent clinical data suggests that COVID-19 is primarily a vascular disease, rather than a respiratory one. This may be due to increasing bradykinin levels, which also increase vascular permeability, in particular in the lungs, and lead to the lungs filling with fluid, immune cells leaking out into the lungs and ultimately, alveolar inflammation. In addition, increased bradykinin levels result in build-up of hyaluronic acid (HLA) in the lungs and this may explain why ventilation is less effective for many COVID-19 patients: since the alveoli in the lungs are filled with HLA hydrogel, oxygen uptake is severely decreased.
The bradykinin hypothesis also accounts for COVID-19’s neurological effects, which include dizziness, seizures, and stroke. MRI studies have revealed that many COVID-19 patients have evidence of leaky blood vessels in their brains.
Calming the bradykinin storm
So what drugs are out there to target the bradykinin system? Currently, there are two approved drugs: icatibant, a B2R blocker, and the monoclonal antibody lanadelumab, which inhibits plasma kallikrein. Both drugs are already being tested in clinical trials for COVID-19. A multicenter randomized clinical trial in the US is testing icatibant in critically ill COVID-19 patients in intensive care and a clinical trial in Cleveland is testing lanadelumab in COVID-19 patients with pneumonia. If these clinical trials show promising results, interventions guided by the bradykinin hypothesis could greatly reduce patients’ suffering and potentially save lives.
References
Garvin et al. (2020) eLife 2020;9:e59177 doi: 10.7554/eLife.59177
